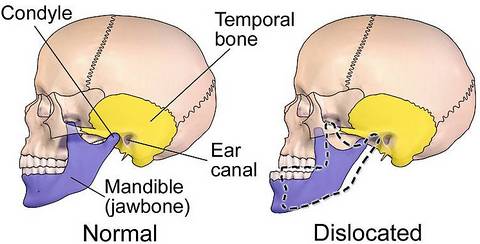
We tend to think of jaw dislocation as confined to a boxing ring but this happens in other sports, or simply due to a face first fall. Dislodging the ball of the joint from the socket in the temporal bone.
Through manipulation, or surgery when essential, the temporomandibular joint can be returned to its rightful position. Ready to bear the strain of the varied movement we are capable of.
Related areas may require treatment, such as the articular disc, which can become displaced, or deteriorate. This could also require care without dislocation, as can other issues which affect the jaw region.
Accurate diagnosis is the key to successful treatment. A combination of digital imaging, tissue, or blood analysis and a maxillofacial consultant’s experience, to identify a range of jaw disorders.
Prevalent Jaw Conditions
Rheumatoid arthritis is a notable cause of jaw pain, an autoimmune, inflammatory disease which can bring swelling and discomfort.
The movements we need to make, such as chewing, or speaking can heighten these symptoms. Ear ache is quite common, or the bodily balance system we have can be out of kilter, causing dizziness, or nausea.
Osteonecrosis is a fairly rare, although damaging condition. The bone degenerates due to lack of blood flow to support the natural renewal process. Alongside, pain, or numbness, your jaw can fail to heal after trauma, or dental work.
Cancer of the jaw can originate in the mouth, or elsewhere and bring similar symptoms. Identifying this at the earliest stage possible is vital for a good long term outcome.
To conditions above, we could add traumatic injuries, fractures, or dislocation. Wisdom teeth have an impact on the jaw, as can infection, the area at the centre of our wellbeing has a range of vulnerabilities.
A Rounded View On Treatment
The likelihood is that one condition lies at the root of unwanted symptoms in the jaw, although making this assumption may not be helpful.
Your consultant should discuss issues you have in detail and carry out a thorough physical examination. They might organise scans of the region, or other tests. Complete understanding leads to good treatment planning.
Whether treatment at our London clinic is for a prevalent jaw disorder, such as temporomandibular joint problems, or a rarer condition, you can be assured this will be based on appreciating your individual needs.
Jaw issues are well understood by specialists and a range of treatment is available. This could be injections, or medication, to ease discomfort and at times, offer a long term solution.
Physical intervention may be needed, from removing fluid, or foreign matter from a joint, to operating on bones, or other tissues, to completely replacing jaw joints with a man made alternative.
The latter is rare and a careful approach may avoid significant surgery. Our team are there to find the best way to restore normal life, without unwanted intrusion.
- Make an appointment
- Phone – 020 7935 8627
- Email – pa@shakib.org


