A Structure We Depend On
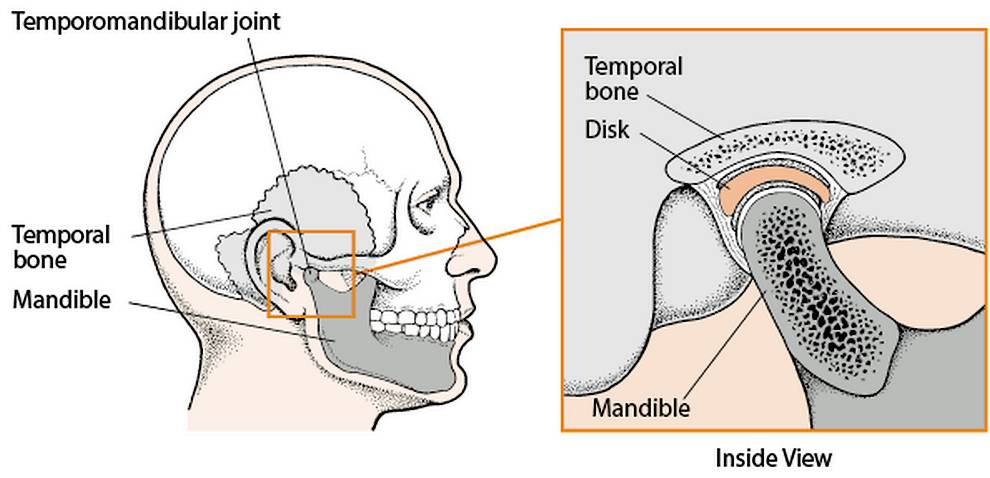
The temporomandibular is a small joint by the front of the ear, where the lower jaw and skull meet. The joint allows your jaw to move and as the image above shows, this is more than a simple ball and socket.
The joint can be damaged, as can the cartilage (articular disc) which acts as a cushion within the joint. Muscles and ligaments which assist the joint can contribute to temporomandibular joint (TMJ) disorder.
The area of jaw disorder is a notable part of oral medicine, such as orthognathic surgery, to correct the position of your jaw where required.
This section focuses on the diagnosis and treatment of TMJ disorder, a condition which 1 in 10 people will face during their lifetime.
Causes & Symptoms
You are welcome to see a little more detail on how this vital joint works and a demonstration of normal movement.
Interference can come from a mild condition, called temporomandibular joint dysfunction, which often improves with rest and lifestyle changes. Treatment may still be required, depending on progress.
A range of conditions can be more serious for the temporomandibular joint. Dislocation, or other abnormal relationships between the disc and articular surfaces are common but not alone in causing issues.
Trauma can be created, by tooth grinding, or clenching. Overloading the jaw, or your chewing muscles might be a contributor, one cause of damage to the articular disc.
External trauma can reduce the joint’s function, or nearby fractures have an indirect effect. Inflammation could arise from other medical conditions, or be related to arthritis.
That could be a form which develop quickly and leaves deposits on joints, or more prevalent conditions, such as rheumatoid arthritis, or degenerative osteoarthritis.
TMJ disorder is likely to be an unpleasant issue, with pain in the muscles, jaw joint, face, or neck. Jaw stiffness, or restricted movement, clicking, or popping sounds, more rarely swelling by the joint.
Although natural misalignment is not usually a root cause, how your upper and lower teeth come together can change due to joint dysfunction. Headaches, hearing loss, or tinnitus are other common side effects.
The causes of temporomandibular joint problems can also be multi-factorial. An accurate assessment is critical for successful treatment to eliminate symptoms.
Professional Diagnosis
Our maxillofacial consultant will carry out a detailed oral examination. Panoramic x-rays, or other specialist imaging techniques may be helpful, to define the detail of your jaw, joints and soft tissues.
Your medical history, perhaps family medical history may be discussed, genetic factors can have a relationship with TMJ disorder.
Issues such as mouth sores, gum disease, sinus function, or unexplained toothache should be investigated. As should previous trauma to the face, or jaw, including biting hard, or unusually wide mouth opening.
Your jaw joints and nearby areas can be examined for pain, clicking, popping, or grating, your bite and facial muscle function analysed.
Jaw problems can create stress, tension, headaches, or shoulder pain. Symptoms which deserve investigation in their own right and are quite common in relation to TMJ disorders.
For such a vital function, examining multiple potential causes helps to ensure that decisions on treatment are the right ones for you.
A Range Of Treatment
Your examination, imaging if carried out and your consultant’s experience help to create a precise treatment plan. The ethos of our clinic is to minimise surgery, we often manage TMJ symptoms conservatively.
Relaxation techniques can assist, or dietary changes, or physiotherapy on the jaw joint. Stopping jaw clenching, grinding, or nail biting could address the problem.
A clear plastic splint is available to fit over your teeth, worn mainly at night, to support the temporomandibular joints and decrease grinding, or pressure.
A procedure called occlusal equilibration can be used, gentle reshaping of the biting surfaces of individual teeth, to create a more even bite. Other dental work can achieve bite balance, such as replacing missing teeth.
Antidepressant medication may be assistive, not simply because stress, or psychological factors could be involved. This type of medication has a muscle relaxing and pain killing effect.
Surgery is available but only suits a proportion of cases. The surgery can simply be steroid injections into the joint, washing the joint out with sterile fluid, eliminating tissue adhesion, or dislodging a stuck cartilage disc.
Significant open joint surgery is rarer. Only likely if bones within the jaw joint are notably deteriorating, a tumour is found to be a cause, or severe scarring, or bone chips lay inside the joint.
Surgery can include replacing the joint with a modern implant, although that should only be considered where damage, injury, infection, or ongoing pain can not be solved in other ways.
Your consultant will advise on procedure if significant surgery is needed and discuss this thoroughly. Even in expert hands, open joint surgery brings a greater healing time and some possibility of nerve injury.
Care At Our London Clinic
Seeing a leading maxillofacial consultant is a sound first step. There may be causal, symptomatic, or separate oral conditions to be addressed. These can be accurately diagnosed and treated.
A complete range of possible jaw conditions will have been considered where your case requires this, to ensure sound treatment planning.
Where a temporomandibular joint disorder is the primary issue, you will receive excellent care, with your treatment focused on minimum intervention for maximum effect.
We appreciate the loss of function and pain TMJ disorders can bring. Issues are not often confined to the jaw itself, discomfort can be wider and core functions such as eating, or speaking are affected.
Good oral function is an essential part of enjoying a healthy, pleasant life. If our London clinic can help, please get in touch with our friendly team.
- Make an appointment
- Phone – 020 7935 8627
- Email – pa@shakib.org


